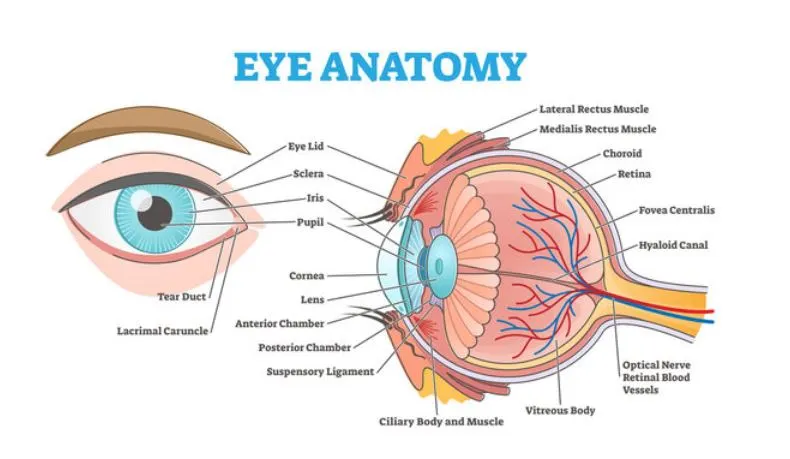
Knowing the anatomy of the eye is critical when you or a near one is deciding whether to go for any sort of surgical procedure. Being aware of how various parts of the eye operate together in sync and how a particular procedure affects them is necessary to make a sound judgement. To help you make a decision that works in your favor, here’s a tour of the main parts of the eye, impacts of ailments/trauma, along with which procedures deployed for treatment.
Cornea
The front part of the eye is known as cornea which is a transparent dome and does most of the focusing of the incoming light. Due to its exposure and a stratified structure, cornea diseases (e.g. thinning, scarring or non-shapely appearance) directly influence vision but can be cured with cornea-directed procedures. One of the most common surgical interventions is Corneal Graft (transplant) to replace tissue that is permanently damaged and Keratoconus and CXL (collagen cross-linking) to prevent further thinning.
Lens
The crystalline lens fine tunes focus but with age or conditions like diabetes and certain autoimmune disorders, it becomes cloudy. This eye condition is known as Cataract, which is mostly treatable with a minor procedure. Cataract surgery (with or without an intraocular lens implantation) or Refractive Lens Exchange (RLE) substitutes the lens in order to restore visual acuity and treat refractive farsightedness.
Iris & Pupil
The amount of light which enters the eye is regulated by the iris. Nearby structures regulate the fluid production and drainage. This is a critical part of the eye that needs to be evaluated before most procedures, as it can temporarily affect intraocular pressure or inflammation.
Retina, Macula & Optic Nerve
These tissues help convert focused light into electrical signals and transmit these signals to the brain. Most front-of-eye operations enhance the picture that is transmitted to the retina, but it is crucial to note that retinal illness may restrict visual performance. This is why the assessment of retina’s health and performance is a critical part of the examination conducted before a surgical procedure.
How each procedure matches anatomy?
The process involves removing the natural or cloudy lens and substituting it with an intraocular lens, to ensure that one sees clearly and, in most cases, does not need glasses.
This implant is inserted in between the natural lens and the iris but does not disturb the natural lens as it is quite thin. It is an additive procedure for patients with high prescriptions or thin corneas and therefore completely not suitable to undergo corneal laser surgery.
Laser Eye Surgery (LASIK/SMILE/PRK)
Laser eye surgery helps reshape the cornea’s surface or internal layers to alter how light is focused onto the retina. Corneal thickness, shape and whether or not the patient has dry eye are necessary assessments to conclude eligibility for this procedure.
Vision Correction Surgery (umbrella term)
This procedure covers corneal laser surgeries, ICLs and lenses-based (RLE). The decision to conduct it is based on anatomy and the assessment usually begins with the corneal health and thickness, age, and the presence of cataract that may have already caused significant damage.
Keratoconus & CXL
Keratoconus is progressive corneal thinning along with cornea turning into a cone-like shape. CXL deploys riboflavin (vitamin B2) and UV light for strengthening the corneal collagen. This combination of therapy usually helps stop the progression of thinning. However, in advanced cases, there might be a need to administer corneal graft.
Corneal Graft (keratoplasty)
This treatment involves the replacement of the diseased corneal tissue with donor tissue to combat dystrophy, scarring, infection or severe thinning, since such conditions cannot be managed with other forms of treatments.
The relevance of anatomy to outcomes & safety?
During pre-operative examination anatomy helps trace danger and probable advantage: corneal topography and corneal thickness, lens clarity, retinal wellbeing and tear danger, and surface dryness. That is why two patients with the same prescription can receive different recommendations. A customized strategy minimizes unexpected events and optimizes the foreseeable conditions.
Patient Expectations
Tests (refraction, corneal topography, pachymetry, lens assessment, retinal exam and in some cases OCT imaging) will be ordered by your surgeon. The recovery period differs: the benefits of corneal laser treatment are usually seen in a few days; while ICL and lens surgeries require several days and weeks of regular check-ups. Antibiotic/anti-inflammatory drops, precautions in terms of activities, and follow-up are the common post-op care guidelines that patients should follow.

Appreciate it for all your efforts that you have put in this. very interesting information.